
The pressure field is a paradigm for understanding and managing patient haemodynamics to optimise end-organ perfusion.
Insights
The pressure field paradigm is based on three insights.
Current haemodynamic monitoring tools don't enable easy identification of haemodynamic phenotype (the patient with an elastic heart versus the patient with undetected heart failure).
Current reference ranges for haemodynamic values (CO, SVR, SV) don't reflect the normal haemodynamics of most patients and aren't good targets.
Measuring and managing vascular tone is as important as measuring and managing cardiac performance - and both CO and SVR are time-averaged values and conceal beat-to-beat performance.
Elements of the pressure field paradigm
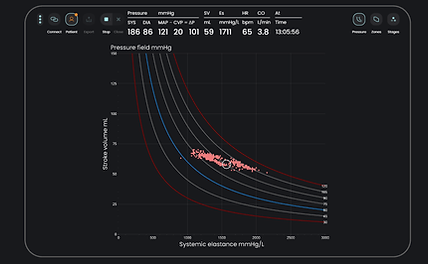
The pressure field graph is a real-time, integrated visualization of the beat-to-beat contributions of the heart and vascular tone to generation of blood pressure. The pressure field software enables real-time display of this graph and supporting information. This enables identification of haemodynamic phenotype, individualised target zones, and tracking of beat-to-beat real-time responses to fluids, pressors, and inotropes.
Interacting with the pressure field software in managing 1,000+ patients during surgery and intensive care has led to the development of a simple management algorithm for patients with a vascular or intermediate phenotype. The goal is to defend a patient's 'normal pressure field zone'. Vasopressors are preferentially used to manage vascular tone - and vasopressors and inotropes are preferentially used to manage SV if there are no signs of hemorrhage. This algorithm is currently being validated.