top of page

The pressure field is a paradigm for understanding and managing patient haemodynamics to optimise end-organ perfusion. The ''pressure field software' enables clinicians to apply the paradigm
How the pressure field helps
The pressure field empowers individualised care by showing real-time responses to fluids, vasopressors, and inotropes, revealing what each patient truly needs.
Clinicians can visualize in real-time whether therapies are working, monitor distance from personalised targets, and guide treatment toward optimal physiologic states.
This new approach replaces reacting to numbers with active management of personalised physiology, powered by a holistic, real-time view of the entire circulation: pressure, flow, and resistance.
Challenges clinicians face
Clinicians today face significant challenges in managing the circulation effectively because practice remains heavily weighted toward pressure monitoring, with limited insight into flow and almost no visibility into resistance.
Although maintaining a MAP above 65 mmHg has become a core tenet of critical care, it often fails to prevent complications or ensure adequate end-organ perfusion, especially in perioperative and septic patients. High-risk OR and ICU patients clearly benefit from individualized hemodynamic management, yet their responses to fluids and pressors remain difficult to predict or assess in real time. This problem is compounded by the fact that clinicians must manage a macro-circulatory system to influence a micro-level process—mitochondrial perfusion—that cannot be directly seen or measured.
As a result, hemodynamic therapy is frequently sub-optimal, particularly for patients at physiologic extremes such as the elderly, the very young, overweight individuals, and small or frail patients. Ultimately, clinicians are forced to treat what they cannot see: current systems do not visualize individual physiologic differences or provide meaningful insight into how patients uniquely respond to therapy.
Elements of the pressure field paradigm and software
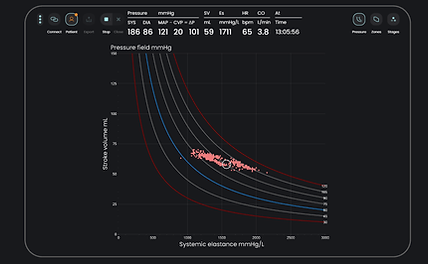
The pressure field graph is a real-time, integrated visualization of the beat-to-beat contributions of the heart and vascular tone to generation of blood pressure. Stroke volume is the contribution of the heart, and systemic elastance is the contribution of the vascular tone. Elastance is a more sensitive measure of vascular tone than SVR and is based on Otto Frank's work with pressure-volume loops.
The pressure field software enables real-time display of this graph and supporting information. This enables identification of haemodynamic phenotype, individualised target zones, and tracking of beat-to-beat real-time responses to fluids, pressors, and inotropes.
Interacting with the pressure field software in managing 1,000+ patients during surgery and intensive care has led to the development of a simple management algorithm for patients with a vascular or intermediate phenotype. The goal is to defend a patient's 'normal pressure field zone'. Vasopressors are preferentially used to manage vascular tone - and vasopressors and inotropes are preferentially used to manage SV if there are no signs of hemorrhage. This algorithm is currently being validated.
How the pressure field helps with specific challenges
Difficulty managing overweight patients. Clinicians often struggle to determine appropriate dosing, fluid needs, and hemodynamic targets in patients with higher body mass. The pressure field provides physiologic insight that helps tailor dosing, fluid strategies, and hemodynamic goals for patients with higher body mass, reducing guesswork.
Difficulty managing small or frail patients. Low-reserve patients can be highly sensitive to therapy changes, making it challenging to titrate fluids, pressors, and inotropes safely. The pressure field helps clinicians fine-tune therapies for vulnerable, low-reserve patients who may be more sensitive to volume, pressure, and medication changes.
Hard to visualize meaningful physiologic differences between patients. Clinicians frequently rely on population norms because individual physiologic variability is not easily visible in real time. The pressure field reveals individual variability in circulation and responsiveness, enabling more personalized care rather than relying on population-based norms.
Difficulty managing older patients with age-related physiologic changes. Age alters responsiveness to fluids and vasoactive medications, complicating the ability to deliver safe, personalised therapy. The pressure field assists in adapting therapies to age-related changes in physiology, supporting safer titration of fluids, pressors, and inotropes.
Uncertainty about the right amount of inotropes a patient truly needs. Without clear feedback on contractility and output, clinicians may overtreat or undertreat when adjusting inotropic support. Shows real-time contractility and perfusion changes in response to inotropic support, reducing overtreatment and undertreatment.
Challenges maintaining consistent end-organ perfusion. Subtle declines in perfusion can go unnoticed, increasing the risk of organ injury before interventions are made. The pressure field highlights when organs may be under-perfused and guides interventions to restore optimal pressure–flow balance.
.
Uncertainty about correct vasopressor dosing for individual patients. Clinicians must balance perfusion pressure against excessive vasoconstriction, often without real-time clarity on patient response. The pressure field monitors how vasopressors affect resistance and flow, helping clinicians avoid harmful over-constriction while ensuring sufficient perfusion pressure.
Difficulty determining the right amount of fluid a patient needs. Assessing fluid responsiveness remains challenging, leading to risks of fluid overload or inadequate volume resuscitation. The pressure field provides immediate feedback on fluid responsiveness and tolerance, promoting precise volume optimisation and reducing fluid overload.
bottom of page